
Healthcare-Related Trauma Counseling and Consulting
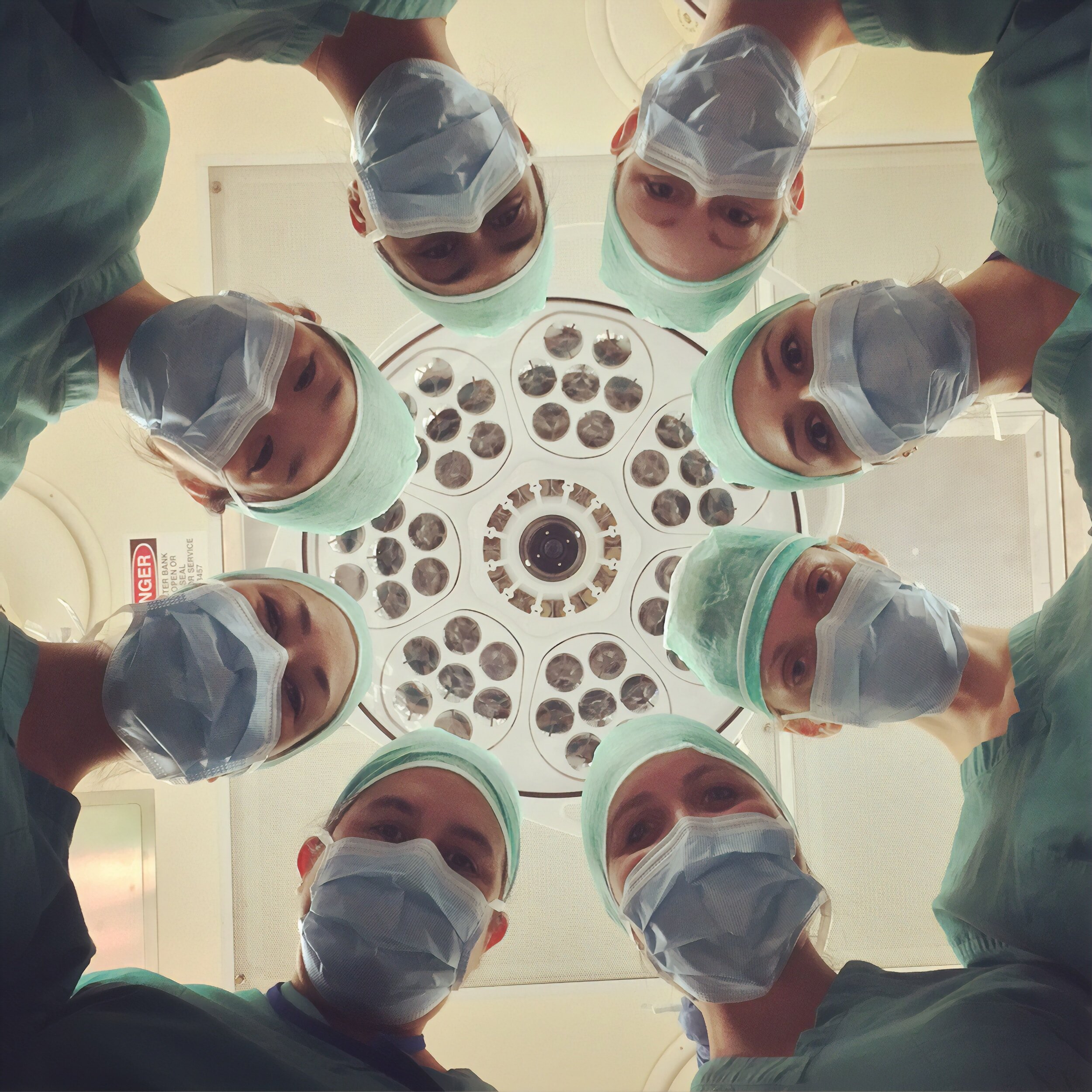
At some point, everyone will have an interaction in the medical system. Unfortunately, sometimes it is through the very act of being healed that a person may experience trauma. Similarly, the healer themselves can experience trauma in moments of intense distress.
I help healthcare providers, educators, and clinicians find ways to prevent and respond to medical trauma in a safe and effective manner and work with clients who struggle with the effects of trauma related to healthcare.
Healthcare-Related/Medical Trauma FAQs
-
Medical trauma refers to the psychological and physiological reactions to injury, diagnosis, illness, and/or treatment of a medical condition. It is experienced by the individual at the center of the medical issue(s) and by the family system and social context in which the individual operates. As with any other traumatic event, all who are involved or connected have their own experience with their own traumatic imprints.
-
Medical trauma actually describes a specific type of trauma that comes interaction with the medical setting. It’s important to distinguish medical trauma from other types of trauma or PTSD because the symptoms can differ. Specifically, the “re-experiencing” criteria we use for assessment for trauma often can be intrusive thoughts that are future-oriented around fears of recurrence and future medical experiences that are possible and sometimes even likely. The other issue with medical trauma that does separate it from other types of trauma that we often see in clinicial environments is that medical trauma can be the result of a procedure or treatment that was done with all good intent and to the best ability of everyone involved. So many other traumas come from people behaving badly, medical trauma can still be present when everyone did their best and the result was “good.” For example, a cancer that is caught early, treated and cured is a positive outcome, but the person who experienced that can still be left with medical trauma. Just because the body has healed and/or “saved” doesn’t mean there are not still mental health implications. Because the health of the body often trumps mental health in medical situations, patients can be left without any language or space to deal with lasting trauma symptoms. As clinicians, if we can be familiar with the specifics of medical trauma, it allows us to further understand, assess, and treat all of our clients.
-
Medical trauma symptoms can vary greatly but typically trauma responses such as negative reactivity to reminders of the medical event, nightmares, panic at the thought of followup care, and feeling shut down or numb when thinking about a difficult medical event could all be symptoms of medical trauma.
-
Awareness starts the process of change. Learning about medical trauma allows us to have language to describe experiences. Finding ways to prevent medical trauma in your own setting can be difficult, so contacting a professional to help can take the burden off of you. Contact me for more information on how I can help you!
-

Professional Education
Elizabeth has spoken to audiences at regional, national, and international levels. She enjoys learning and sharing knowledge with other professionals, approaching opportunities with humor and warmth. Elizabeth is available for both virtual or in-person trainings.
-
Consulting Services
Elizabeth provides personalized consultation services to better equip systems to prevent and respond to medical trauma including assessment of policies and procedures and formal recommendations.
-

Clinical Consultation
If you are a mental health clinician and would like to receive professional consultation on working with clients who experience medical trauma, Elizabeth is available for either virtual or inperson consultation sessions.
Let’s work together.
Let me know how I can assist you in working to understand and prevent Medical Trauma.
